Taking opioids in combination with other central nervous system depressants—like benzodiazepines, alcohol, or xylazine—increases the risk of life-threatening overdose.1,2 Learn more about the effects of taking more than one type of drug (polysubstance use) from the U.S. Centers for Disease Control and Prevention (CDC).
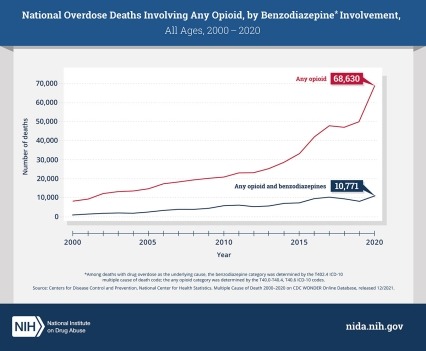
In 2021, nearly 14% of overdose deaths involving opioids also involved benzodiazepines, a type of prescription sedative commonly prescribed for anxiety or to help with insomnia.3 Benzodiazepines (sometimes called "benzos") work to calm or sedate a person, by raising the level of the inhibitory neurotransmitter GABA in the brain. Common benzodiazepines include diazepam (Valium), alprazolam (Xanax), and clonazepam (Klonopin), among others.
Researchers have also found benzodiazepines in the illicit opioid supply in some areas, which may mean that people are taking benzodiazepines in combination with illicit opioids knowingly or unknowingly.2
Co-Prescribing Opioids and Benzodiazepines
Every day, approximately 220 Americans die after overdosing on opioids.3 Combining opioids and benzodiazepines can increase risk of overdose because both types of drugs can cause sedation and suppress breathing—the cause of overdose fatality—in addition to impairing cognitive functions. Research shows that people who use opioids and benzodiazepines concurrently are at higher risk of visiting the emergency department, being admitted to a hospital for a drug-related emergency, and dying of drug overdose.4,5
For example, a cohort study in North Carolina found that the overdose death rate among patients receiving both types of medications was 10 times higher than among those only receiving opioids.6 A study among U.S. veterans with an opioid prescription found that receiving a benzodiazepine prescription was associated with increased risk of drug overdose death in a dose-dependent manner.7
The Centers for Disease Control and Prevention (CDC) Clinical Practice Guideline for Prescribing Opioids for Pain recommends that clinicians use particular caution when prescribing benzodiazepines concurrently with opioids and consider whether benefits outweigh risks.8 Both prescription opioids and benzodiazepines now carry U.S. Food and Drug Administration boxed warnings on their labels highlighting the potential dangers of using these drugs together.
People being prescribed any medication should disclose all other substances and medications they use and consult with their health care teams about avoiding or managing the risks of using certain medications and substances in combination.
References
- Liu S, O'Donnell J, Gladden RM, McGlone L, Chowdhury F. Trends in nonfatal and fatal overdoses involving benzodiazepines—38 States and the District of Columbia, 2019-2020. MMWR Morb Mortal Wkly Rep. 2021;70(34):1136-1141. Published 2021 Aug 27. doi:10.15585/mmwr.mm7034a2
- Laing MK, Ti L, Marmel A, et al. An outbreak of novel psychoactive substance benzodiazepines in the unregulated drug supply: Preliminary results from a community drug checking program using point-of-care and confirmatory methods. Int J Drug Policy. 2021;93:103169. doi:10.1016/j.drugpo.2021.103169
- CDC WONDER. Multiple Cause of Death 1999-2021. Centers for Disease Control and Prevention, National Center on Health Statistics. Released January 2023. Accessed January 2023.
- Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996-2013. Am J Public Health. 2016;106(4):686-688. doi:10.2105/AJPH.2016.303061
- Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356:j760. Published 2017 Mar 14. doi:10.1136/bmj.j760
- Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17(1):85-98. doi:10.1111/pme.12907
- Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ. 2015;350:h2698. Published 2015 Jun 10. doi:10.1136/bmj.h2698
- Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC clinical practice guideline for prescribing opioids for pain — United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1–95. doi: 10.15585/mmwr.rr7103a1