Highlights
Image

NIDA Image
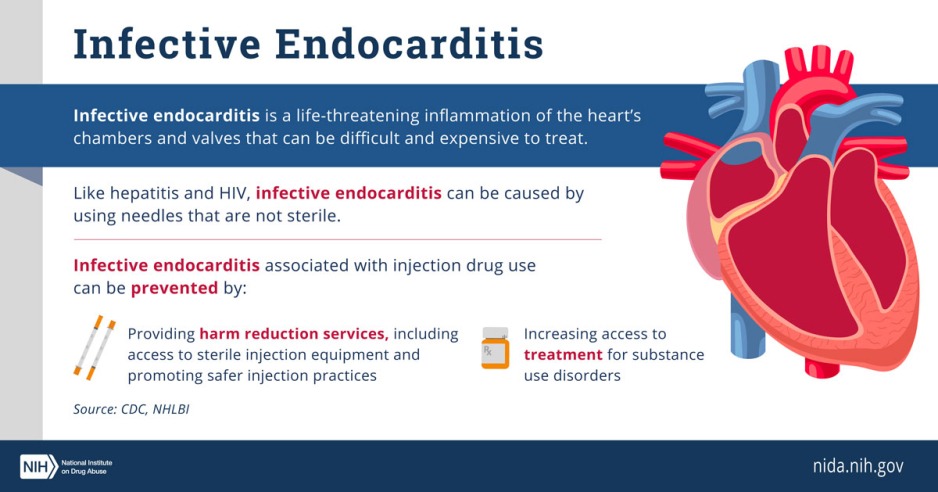
- Syringe services programs (SSPs) are community-based prevention programs that can provide a range of services, including access to and disposal of sterile syringes and injection equipment, vaccination, testing, and linkage to infectious disease care and substance use treatment. Nearly 30 years of research show these programs are safe, effective, and cost-saving tools that can prevent HIV and high-risk injection behaviors among people who inject drugs.
- Syringe services programs help protect communities by preventing infectious disease outbreaks and facilitating safe disposal of used syringes. These programs are not associated with increased drug use, crime, or syringe litter in communities.
- The most effective syringe services programs provide comprehensive services to people who inject drugs, including the distribution of lifesaving medications and referrals to substance use treatment and other health care.
Latest from NIDA
Syringe services for people who inject drugs are enormously effective, but remain underused
|
December 1 is World AIDS Day, an opportunity to underscore the solid science behind syringe services programs
Improving community engagement in addiction science
|
NIDA is committed to improving community engagement in all parts of the research process
Federal study examines care following nonfatal overdose among medicare beneficiaries; identifies effective interventions and gaps in care
|
Receiving gold-standard care after a non-fatal overdose was associated with a decreased risk of subsequent overdose.
Find More Resources on Syringe Services Programs
- Learn more about Syringe Services Programs from the CDC.
- Learn more about Syringe Services Programs and HIV from HIV.gov.
- Learn more about harm reduction strategies to lessen HIV risks from the National Institute of Allergy and Infectious Diseases.