A cross-country group of researchers funded by NIDA has identified needed areas of research related to the intertwining epidemics of HIV, COVID-19 and the increasing use of methamphetamine in the United States among men who have sex with men. The authors suggest that co-occurring methamphetamine use and HIV present compounded risk for contracting the novel coronavirus (SARS-CoV-2), helping to fuel the current COVID-19 pandemic.
The prevalence of stimulant use is two-fold greater among men living with HIV, which can undermine the benefits of key HIV prevention strategies, including the approach known as “Undetectable Equals Untransmittable,” or U=U, that focuses on immediately treating people living with HIV with anti-retroviral therapies and keeping them engaged in care and virally suppressed to undetectable levels to prevent HIV transmission. Moreover, because methamphetamine use has been consistently linked to sexual risk taking behaviors among men who have sex with men it may also lead to difficulties adhering to COVID-19 social distancing guidelines.. The COVID-19 pandemic also is a chronic uncontrolled stressor and can exacerbate drug use and associated risk factors.
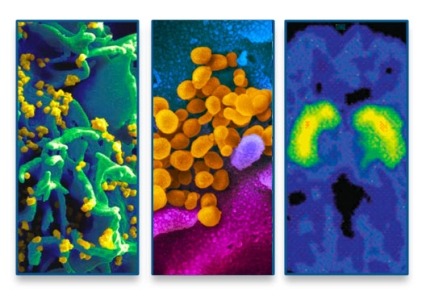
The authors suggest that these co-occurring public health crises threaten to compromise the benefits of HIV treatment and increase biological vulnerability to SARS-CoV-2 infection. For example, HIV damages the immune system even when people are virally suppressed, a phenomenon referred to as residual immune dysregulation. Prior findings from the research team demonstrate that methamphetamine use could exacerbate this damage even in those receiving effective HIV treatment. Together, HIV and methamphetamine use could set the stage for SARS-CoV-2 infection by amplifying immune damage.
Research has shown that people living with HIV who use stimulants experience profound difficulties with navigating the HIV care continuum, including poorer adherence to anti-retroviral therapy, resulting in slower rates of viral suppression, contributing to increased mortality. With treatment and services even harder to access during the COVID-19 crisis, the authors suggest there is a clear need for scalable, mHealth interventions to address the psychiatric burden of the pandemic.
To halt community-level transmission of SARS-CoV-2, the authors highlight the need to understand the bio-behavioral mechanisms that could account for the potential exacerbated risk experienced by those living with co-occurring methamphetamine use and HIV. This will require a sustained, coordinated response that integrates behavioral and biomedical approaches much like we have witnessed in over three decades of the HIV epidemic.
Study:
- Adam W Carrico, Keith J Horvath, Christian Grov, Judith T Moskowitz, Savita Pahwa, Suresh Pallikkuth, Sabina Hirshfeld. Double Jeopardy: Methamphetamine Use and HIV as Risk Factors. AIDS and Behavior.
