Studies found:
- The spread of marijuana use and the opioid epidemic over the past 10 years have affected middle-aged and older Americans.
- Prescription opioid and benzodiazepine misuse increased older adults’ risk of suicidal thoughts.
Three recent NIDA-supported studies highlight the importance of screening older adults for drug use and its consequences. Researchers demonstrated steep rises in marijuana use among middle-aged and older Americans, and prescription opioid misuse and heroin use among older Americans. The researchers also documented widespread polydrug use among older people who use marijuana and increased suicidal ideation among those who misuse prescription opioids.
More Middle Aged and Older Adults Use Marijuana
Inquiries about marijuana from older patients prompted Drs. Benjamin H. Han and Joseph J. Palamar of New York University to quantify trends in middle-aged and older Americans’ use of the drug. The investigators analyzed data from the National Survey on Drug Use and Health (NSDUH), which annually asks approximately 70,000 Americans of all ages about their drug use and other health-related issues. They found that in the 2015–2016 NSDUH, 9 percent of respondents age 50 to 64, and 2.9 percent of those age 65 and older, reported using marijuana during the past year. Those percentages represented increases of 27 percent and 107 percent compared with the 2012–2013 NSDUH; and 100 percent and 625 percent compared with the 2006–2007 survey.
The researchers’ analysis pointed to evolving perceptions about marijuana’s dangers and potential medical uses as contributing to middle-aged and older adults’ rising use. A large majority of both age groups indicated that they felt that using the drug as often as twice weekly conferred slight or no risk of bad consequences. Moreover, 15 percent of adults age 50 to 64 and 23 percent of adults age 65 and older reported that they had used the drug with a doctor’s recommendation.
In the 2015–2016 NSDUH, marijuana use was three times as prevalent in those age 50 to 64, compared with those age 65 and older. The researchers suggest that this could partly reflect the younger group’s having had more experience with marijuana as teenagers. More than 80 percent of respondents age 50 to 64 had tried marijuana by age 19, compared to slightly more than half of those age 65 and older. Overall, respondents who reported marijuana use before age 19 had a 13-fold increase in their odds for being current marijuana users.
Additional analyses showed that older marijuana users had twice the odds of alcohol use disorder, nearly 8 times higher odds of cocaine use, and twice the odds of prescription opioid misuse, compared with nonusers of the drug. Older marijuana users also were more likely to be dependent on nicotine and to have had major depression in the past year.
More Older Adults Enter Treatment for Opioid Use Disorder
Older Americans have not been spared in the ongoing epidemic of opioid use and misuse, Dr. Andrew S. Huhn and colleagues at the Johns Hopkins School of Medicine report. The researchers tracked the trend in first-time treatment admissions of U.S. adults age 55 and older with a primary diagnosis of opioid use disorders, as recorded in the Treatment Episode Data Set, from 2004 to 2015. The number climbed roughly 8 percent annually from 2004 to 2012, then surged 25 percent each year from 2013 to 2015. Across the years 2004 to 2015, it increased from roughly 10 percent to more than 20 percent of all first-time treatment admissions in this age group (see Figure 1).
Dr. Huhn calls one of his team’s findings, in particular, “incredibly alarming”: Between 2012 and 2015, the number of first-time admissions of U.S. adults age 55 and older who were using heroin doubled, from 2,725 to 5,636. In fact, heroin users accounted for almost the entire doubling of opioid treatment admissions in this population in those years. ”We did not expect to see heroin use at this level,” says Dr. Huhn. Moreover, the prevalence of intravenous heroin administration in the older adults was greater, at 49 percent, than that among those under age 55.
Further analyses revealed that, compared with younger age groups, older adults entering treatment for heroin use were more likely to be male, black or African American, retired, and living in urban areas. “Identifying these trends should inform public health efforts to effectively engage and treat this population,” says Dr. Huhn.
Prescription Drug Misuse Linked to Suicidal Thoughts
Among the many adverse consequences of prescription opioid misuse by older Americans is an increased prevalence of suicidal ideation, according to a recent study by Dr. Ty S. Schepis from Texas State University and his colleagues from the University of Maryland and the University of Michigan. Older Americans, especially men, already are more likely than the general population to think about suicide; the researchers showed that prescription opioid misuse increases their risk still further.
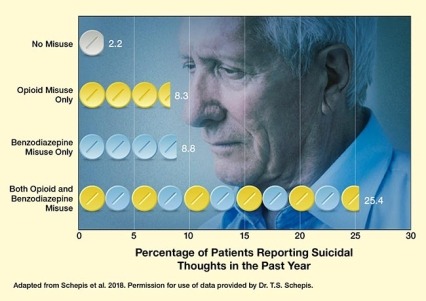
Dr. Schepis’ team analyzed data from the adults age 50 and older who participated in the 2015–2016 NSDUH. Those who misused both prescription opioids and benzodiazepines were 10 times more likely than those who did not to report that they “thought seriously about killing” themselves during the past year (see Figure 2). Appropriate use of these medications, in contrast, was not associated with increased thoughts of self-destruction.
See full text description at end of article.
Calls for Vigilance, Proactivity, and More Research
Dr. Han and colleagues say their findings highlight the importance of screening middle-aged and older adults for marijuana use, and, among those who use the drug, for related behavioral health problems and consequences. In addition, says Dr. Han, health care providers and other stakeholders must develop tools to engage older adults in treatment; coordinate care between addiction specialists, primary care physicians, and other medical specialties; and leverage community services to best support older adults who use drugs.
Given the limited clinical research data on the benefits and risks of marijuana use for older Americans, Dr. Han emphasizes the need for further studies. “This is important to note, as we see dramatic increases in marijuana use by older adults, who often have comorbid chronic conditions and take many prescribed medications, and therefore may be at higher risk of the adverse effects of marijuana use without a clear understanding of its benefits,” he says.
Dr. Schepis’ findings reinforce the importance of screening older adults for use of illicit opioids and remaining alert for signs of potential opioid or benzodiazepine misuse, such as early refill requests or having multiple prescriptions from different doctors. Dr. Schepis and his colleagues recommend that health care providers assess older patients who show such signs for suicidal thoughts.
These studies were supported by NIH grants DA043651 and DA038800 (Han); DA035327 (Huhn); and DA036541, DA042146, and DA043696 (Schepis).
- Text Description for Figure 1
-
The bar chart shows the percentage of patients of two different age groups who entered opioid use disorder (OUD) treatment for the first time for treatment of primary OUD from 2007 to 2015. Red bars indicate values for people under age 55 and blue bars indicate values for people age 55 and older. The red dashed line indicates the trend for people under age 55, and the blue line indicates the trend for people age 55 and older. The horizontal x-axis shows the different years from 2007 to 2015, and the vertical y-axis shows the percentage of patients entering OUD treatment for the first time from 0 percent to 30 percent.
For people under age 55, the percentages of first-time admission to OUD treatment were about 12 percent in 2007, about 13 percent in 2008, about 14 percent in 2009, about 15.5 percent in 2010, about 17 percent in 2011, about 19 percent in 2012, about 21 percent in 2013, about 23 percent in 2014, and about 25 percent in 2015. For this age group, the red dashed line indicates a relatively stable trend in admission increases of about 10 percent per year throughout the entire period.
For people age 55 and older, the percentages of first-time admission to OUD treatment were about 13 percent in 2007 and 2008, about 14 percent in 2009, about 13 percent in 2010 and 2011, about 14 percent in 2012, about 14.5 percent in 2013, about 17 percent in 2014, and about 22 percent in 2015. For this age group, the blue line indicates two trends. From 2007 to 2013, first-time admissions remained relatively stable, but from 2013 to 2015, there was a steep increase in admissions of about 25 percent per year.
- Text Description for Figure 2
-
The horizontal bar chart illustrates the percentage of patients ages 50 and older who reported suicidal thoughts in the past year, based on their misuse of prescription opioids or benzodiazepines. The image in the background shows a sad-looking older Caucasian man. In the graph, the horizontal x-axis indicates the percentage of patients reporting suicidal thoughts in the past year from 0 percent to 30 percent. The vertical y-axis indicates the drug use categories, with a white pill (top row) indicating no drug misuse, yellow pills (second row) indicating prescription opioid misuse only, blue pills (third row) indicating benzodiazepine misuse only, and alternating yellow and blue pills (fourth row) indicating both opioid and benzodiazepine misuse. Percentages of patients reporting suicidal thoughts in the last year were 2.2 percent for those with no misuse of drugs, 8.3 percent for those with misuse of prescription opioids only, 8.8 percent for those with misuse of benzodiazepines only, and 25.4 percent for those with misuse of both opioids and benzodiazepines.
Sources:
- Han, B.H.; Palamar, J.J. Marijuana use by middle-aged and older adults in the United States, 2015-2016. Drug Alcohol Depend. 191:374-381, 2018.
- Huhn, A.S.; Strain, E.C.; Tompkins, D.A.; Dunn, K.E. A hidden aspect of the U.S. opioid crisis: Rise in first-time treatment admissions for older adults with opioid use disorder. Drug Alcohol Depend. 193:142-147, 2018.
- Schepis, T.S.; Simoni-Wastila, L.; McCabe, S.E. Prescription opioid and benzodiazepine misuse is associated with suicidal ideation in older adults. Int J Geriatr Psychiatry. 34(1):122-129, 2019.